
Dr. Deva Boone MD, FACS,FACE
Vitamin D in Parathyroid Disease – The topic that generates the most confusion for parathyroid patients and their doctors is Vitamin D. Some of the interactions and concepts with Vitamin D are complex, but in this blog I hope to highlight a few principles that will help you understand this vitamin and its place in parathyroid disease.
Example – Let’s review a pretty common scenario. Laura is a 54 year old woman recently told by her primary care physician, Dr. Smith, that she has low Vitamin D levels. Dr. Smith knows the importance of Vitamin D, so he prescribes the logical treatment for Vitamin D deficiency: Vitamin D supplementation. If Dr. Smith routinely checks a lot of different labs, he may even notice that Laura’s parathyroid hormone (PTH) level is a little high. Dr. Smith vaguely remembers something from his training about low Vitamin D levels leading to high PTH levels, and concludes that giving large doses of Vitamin D will fix Laura’s PTH levels in addition to her Vitamin D levels.
Common Error – Dr. Smith has just made the most common physician error that I see in treating patients with parathyroid disease. Dr. Smith means well, and a true Vitamin D deficiency can be treated with Vitamin D supplementation. Chronic Vitamin D deficiency can lead to a rise in PTH in certain circumstances. So what was the error?
To understand this, I need to back up a bit, and explain a few things about Vitamin D.
Forms of Vitamin D – There are many different forms of Vitamin D. For our purposes, there are two forms that we need to focus on.
1. 25-hydroxyvitamin D (25-OH Vit D). This form is also called calcifediol or calcidiol – I will generally avoid using these names because they sound so much like “calcium” that it can be confusing. For the rest of the article, this will be called 25-OH Vitamin D or inactive Vitamin D. When your doctor checks your Vitamin D, this is the form that he or she is usually checking (usually not any of the other forms). It can be thought of as the inactive Vitamin D in your body. This is the form that cannot actually do much until it is converted into the active form, which brings us to…
2. 1,25-dihydroxyvitamin D (1,25-diOH Vit D). This form is the active form, and is also known as calcitriol. For the rest of the article, I will refer to this one as 1,25 Vitamin D or the active Vitamin D. This is the form that produces the effects of Vitamin D. When we talk about the role of Vitamin D in the body, we are talking about what this form does.
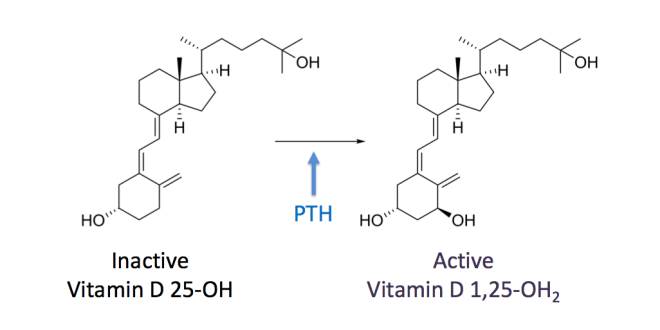
Conversion from Inactive to Active Vitamin D – In your body, you have both inactive and active forms of Vitamin D. As you might guess, the inactive 25-OH needs to be converted into the active 1,25 form. This occurs in the kidneys, by a specific enzyme (it’s called 25-hydroxyvitamin D31-alpha-hydroxylase). The activity level of this enzyme determines how much inactive Vitamin D is converted to active Vitamin D. If the enzyme is sluggish, then not much Vitamin D will be activated. If the enzyme is fired up, then a lot of the inactive form will be converted to the active form. If more active form is created, then you will see more activity of Vitamin D. I will explain that further in a moment.
What determines the activity level of the converting enzyme? – Here is a question with extreme importance, though many doctors do not know or have forgotten the answer: What determines the activity level of that enzyme? Or, put another way, what determines how much active Vitamin D is made? This isn’t just a question for biochemists, because the answer has consequences for every patient with parathyroid disease.
The answer is parathyroid hormone (PTH). PTH essentially “turns on” the enzyme, telling it to speed up and activate more Vitamin D. PTH is made by the parathyroid glands. If your parathyroid glands make more PTH, then more Vitamin D will be activated.
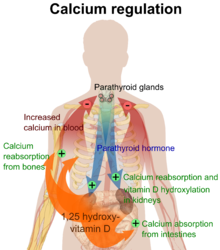
Role of active 1,25 Vitamin D – Now we need to know what active Vitamin D (1,25 Vitamin D) actually does. There are two very important actions of 1,25 Vitamin D:
1. Increase intestinal absorption of calcium
2. Prevent loss of calcium into urine, by increasing the amount of calcium reabsorbed in the kidneys
Both of these actions serve the same purpose, to increase the amount of calcium in the blood.
Recap – Let’s recap the process we have so far: You have a bunch of inactive Vitamin D in your body, but it cannot do anything until it is activated. It has to be activated in the kidneys by a certain enzyme. That enzyme is always working, but will be sluggish until it gets a kick in the pants from PTH. Once PTH stimulates that enzyme, it churns through the inactive Vitamin D to make active Vitamin D. Active Vitamin D then helps your body increase the blood calcium levels.
Function of Parathyroid Glands
Why is PTH in charge of this Vitamin D process? – PTH is in charge because the parathyroid glands are built to regulate calcium. In fact, that is all that the parathyroid glands do: control the calcium levels in the blood. Activating Vitamin D is one of the main ways in which PTH controls calcium levels. The parathyroid glands monitor the amount of calcium in the blood. When the blood calcium level is too low, the parathyroid glands make PTH in order to raise calcium levels. When the calcium level is too high, the parathyroid glands stop making PTH, so the calcium level will fall back down. This happens many times throughout the day, without you even realizing it, and it keeps your calcium in a very tight range – if your parathyroid glands are working normally.
How Parathyroid Tumor Affects The Process – If you have a parathyroid tumor, things are a little different. In this scenario, your overactive parathyroid gland with a tumor is no longer doing its job properly. It’s not carefully calibrating the amount of PTH production based on the current blood calcium level. Instead, it is just making PTH without any consideration to the calcium level. Even as the calcium level gets too high, it keeps making PTH. That PTH is going to continually activate the enzyme that produces active Vitamin D. Active Vitamin D is produced from inactive Vitamin D, so the more that enzyme works, the more active Vitamin D you have – and the less inactive Vitamin D you have.
You can now see why patients with parathyroid tumors have low levels of inactive Vitamin D. All of that form of Vitamin D is being converted to active Vitamin D! If you measure the levels of active Vitamin D in patients with parathyroid disease, you will find that they are usually high.
It’s worth repeating: For patients with parathyroid tumors, the level of active Vitamin D (1,25 Vitamin D) is often HIGH, because the inactive form is being converted into the active form. But this is not the form of Vitamin D that physicians generally measure. Instead, we check the inactive form.
Why is inactive Vitamin D routinely checked rather than the active form? There is a reason why we routinely check the inactive 25-OH form rather than the active 1,25 form.
Levels of the inactive form are more stable over a longer period of time. The active form tends to break down within a few hours, so you are getting a very brief snapshot of Vitamin D status. The inactive form gives a better sense of long-term Vitamin D status in most patients. For those who have normal parathyroid function, the inactive form is really all you need to measure to get a good sense of overall Vitamin D status. But for patients who have a parathyroid tumor, the inactive form is misleading.
Most patients with parathyroid disease have low levels of the inactive form, and are diagnosed with Vitamin D deficiency. If you measured the active form, you would find that most of these patients actually have high Vitamin D (but it is in the active form). It is possible to check the active form in a blood test; your doctor just needs to request the 1,25 dihydroxy Vitamin D specifically. When most doctors order Vitamin D, they will automatically get the 25-OH inactive Vitamin D.
Back to Laura and Dr. Smith – When Dr. Smith found that Laura had a low Vitamin D, what he meant was that she had a low 25-OH Vitamin D, because that is generally what doctors are referring to when they do not specify the form. If Laura has normal parathyroid function, then her active form will also likely be low. If she has a parathyroid tumor, then it is not surprising that she has a low inactive form, because it has been converted to the active form.
Here is the mistake Dr. Smith made: he didn’t check a calcium level before prescribing Vitamin D. If he had, he would have seen that Laura’s calcium level was 10.5 mg/dl, which is high for her age. Combined with an elevated PTH level, we can be certain that Laura has primary hyperparathyroidism, usually caused by a parathyroid tumor. Her parathyroid tumor is acting inappropriately, putting out more PTH than it should be. This is causing the inactive Vitamin D to be converted to the active form. Her active form of Vitamin D is likely high, but no one has checked it.
Should Laura take Vitamin D supplements? Does she need more Vitamin D? No. Recall one of the main roles of Vitamin D: helping to raise the blood calcium levels. Her calcium is already high; she doesn’t need to make it higher. Taking Vitamin D (either D2 or D3, which are both inactive forms) will lead to even higher levels of active Vitamin D (which is already high!) and higher levels of calcium. Meanwhile, the inactive Vitamin D levels will likely remain on the low end – because as soon as it gets in, it is being converted to the active form. Laura needs her parathyroid tumor removed; she does not need Vitamin D.
In Laura’s case, her inactive Vitamin D is low because her PTH is high. The PTH is causing the Vitamin D to be low. But I mentioned earlier that a low Vitamin D could cause the PTH to be high. How do we know that Laura’s low Vitamin D is not causing her PTH elevation?
The answer is the calcium level. If someone has a true Vitamin D deficiency over a long period of time, they will have problems with absorbing calcium in the intestines, since Vitamin D is essential for that. Calcium levels will then run in the low range (usually mid 8s to low 9s in mg/dl). Because the parathyroid glands are sensitive to calcium levels, they will start making more hormone (PTH) when they sense the low calcium. In this scenario, low Vitamin D leads to low calcium, which leads to high PTH levels. If the calcium is high, then low Vitamin D cannot lead to high PTH, and we can assume that the high PTH is the cause of the low Vitamin D, not the other way around.
Another common mistake – Laura’s friend Peter sees Dr. Jones. Peter was also recently told that he had a low Vitamin D level. His physician, Dr. Jones, knew to check a calcium level, and found that it was high. She also found a high PTH. So far she is on the right track. She vaguely remembered a connection between calcium, Vitamin D, and PTH. But she incorrectly concludes that a low Vitamin D level can lead to a rise in PTH, which then raises the calcium level. This is another very common mistake I see. Dr. Jones is now under the impression that she can “treat” the high calcium with Vitamin D supplements. This logic is incorrect, because low Vitamin D causes low calcium, which then causes high PTH levels. If the calcium is high, it will suppress the parathyroid glands and cause them to stop making more PTH, regardless of what the Vitamin D level is. If the calcium is high, and the PTH is also high, then there is a problem with the parathyroid glands. Treating this with Vitamin D is not going to help, and may actually harm the patient, since Vitamin D can raise blood calcium levels that are already high.
A note on Vitamin D supplements – I will not go into whether there is a health benefit to taking Vitamin D supplements, or how much benefit there is. This issue is complicated. Many people do not need these supplements, though many also do. If you are taking Vitamin D supplements, you need to know about the risk of taking high doses. Recall that Vitamin D helps the intestines absorb calcium. High-dose Vitamin D can thus lead to elevated calcium levels. Sometimes I will review the records of a patient with high calcium levels and I will notice that the person is taking 5000 units or more of Vitamin D daily. Some can take this dose safely and have no side effects! But others will get high calcium levels. This confuses the picture and makes it hard to tell whether the high calcium is due to a parathyroid tumor or Vitamin D oversupplementation. If the PTH level is high, then the answer is clear: it is a parathyroid tumor. Patients with Vitamin D oversupplementation and high calcium will have PTH levels that are low or low normal (usually in the 10 to 35 pg/ml range). If you have high calcium and are on high-dose Vitamin D, you should stop now, for two reasons:
1. Vitamin D can raise your calcium further, which can make you feel worse.
2. Vitamin D may be the cause of the high calcium, and stopping it will correct your calcium levels. Note that it may take a few months for your Vitamin D levels to drop sufficiently to see a drop in the calcium. Also remember that if the PTH is high or high-normal, then the problem is not Vitamin D. You should stop taking Vitamin D – and then see a surgeon about getting your parathyroid tumor removed.
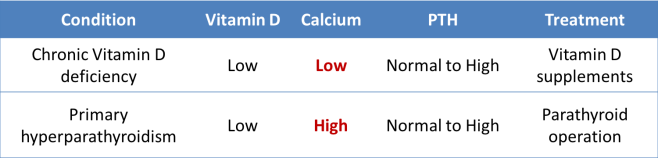
Take-home message – Vitamin D exists in multiple forms, and the one that we commonly measure is the inactive 25-OH form. This is frequently low in patients with parathyroid disease, because PTH drives the conversion of the inactive form into the active form. If you are diagnosed with a Vitamin D deficiency, the first thing to do is check your calcium. If your calcium is HIGH, with a low Vitamin D, then you likely have a parathyroid tumor. You do not need to take Vitamin D – you need to check a PTH level and may need a parathyroid operation. If your calcium is LOW, with a low Vitamin D, then you should take Vitamin D supplements. When taking supplements, be wary of taking high doses without a clear indication, and if your calcium is high, stop taking the supplement.
Learn more about Dr. Deva Boone….
Dr. Deva Boone is the Medical Director of the Norman Parathyroid Center at Tampa General in Tampa, Fl. and is one of seven expert parathyroid surgeons at the high volume center that performs 4000+ parathyroidectomies per year.
After growing up in New Jersey, she attended Cornell University for both her undergraduate degree and medical degree. She then trained in general surgery at St. Luke’s Roosevelt Hospital Center in New York City. While there, she received several awards for research and academic performance, including the highest award for outstanding contributions to surgical education and research. Dr. Boone received additional fellowship training in endocrine surgery at NorthShore University in Chicago. Dr. Boone joined the Norman Parathyroid Center in 2014. Dr. Boone oversees clinical research efforts at NPC and published their largest series of parathyroidectomy patients (over 20,000 from our database). She enjoys surgical missions and has provided surgical care to patients in Nigeria, Myanmar, and the Dominican Republic.

Found this extremely informative thankyou ,recently had 3 p arathyriods out and struggling on calci D considering going back on adcolD3,i don’t think many family Dr understand this illness which make it difficult for us 😕
LikeLike
Glad you found our post informative. It is indeed difficult at times to get family doctors to understand this disease. Best of luck to you!
LikeLike
Thank you for this informative article. I wonder why so many physicians don’t know much about parathyroid although it’s a very important gland.
LikeLike
I took high doses vit D a few years ago before i knew about hyperpara .. i took it because I always felt down in the winter , my levels of calcium & pth were 2.58 2.66 2.4 pth 9 I was admitted to hospital a few times with bad palpitations & tingling around mouth & fingers ….I stopped taking vit d about a year or so ago when i read that it could increase calcium …my last 2 readings were …..calcium 2.4 pth 6 ……then last month calcium 2.53 pth 5. Vit D 53 …so have i overdosed on vit D supplement ?
LikeLike
Based on information shared in the article it is possible to elevate ones calcium by taking too much Vitamin D. A takeaway is that it is important to understand the symptoms of primary hyperparathyroid disease and its various biochemical presentations before starting Vitamin D supplementation for the purpose of trying to manipulate PTH or calcium values. Low inactive Vitamin D is a player in those biochemical presentations.
LikeLike
I am so thankful for this article. After 5 yrs of mysterious elevated liver enzymes, high cholesterol and Osteoporosis, in spite of healthy lifestyle . The Norman Center has been instrumental in requesting my PTH checked by my doctor, since my Ca was 10.3 and Vit D was super low. PTH was off the charts. I will be contacting the Norman Center to become a patient and hopefully get my life back.
LikeLike